The Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) requires that Mental Health and Substance Use Disorder (MH/SUD) treatments provided by managed care organizations (MCOs) have limitations on MH/SUD benefits that are equivalent to those for medical/surgical (M/S) benefits and are applied no more stringently. Provisions of the MHPAEA became applicable to the Oregon Health Plan (OHP) in October 2017 when the Medicaid Parity Final Rule (42 Code of Federal Regulations [CFR] §438 Subpart K) went into effect. The rule requires parity in the following key areas:
- Aggregate lifetime and annual dollar limits (AL/ADLs).
- Financial requirements (FRs—such as copays).
- Quantitative treatment limitations (QTLs—such as day and visit limits).
- Non-quantitative treatment limitations (NQTLs—such as prior authorization [PA] and provider network admission requirements).
Additional mental health parity (MHP) regulations require that criteria for medical necessity determinations for MH/SUD benefits must be made available to beneficiaries and providers upon request, as well as the reason for the denial of reimbursement or payment for MH/SUD benefits. States must also implement monitoring procedures to ensure continued compliance and to identify when changes in benefit design or operations could affect compliance and require an updated analysis. Finally, Oregon House Bill 3046 (HB 3046), enrolled in 2021 and effective in 2022, outlined additional MHP reporting requirements (i.e., MH/SUD and M/S service utilization, adequacy of MH/SUD provider networks, and collaboration with community partners) for Coordinated Care Organizations (CCOs) and OHP Fee-for-Service (FFS), culminating in the presentation of a comprehensive report to the Oregon legislature annually.
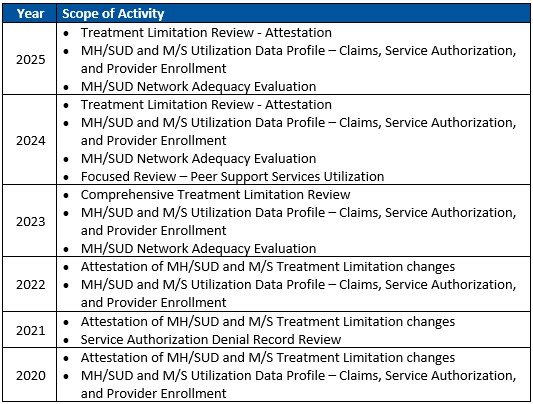
Since 2020, HSAG has conducted an MHP analysis to determine if treatment limitations applied to MH/SUD benefits are compliant with the MHPAEA of 2008 and 42 CFR §438 Subpart K. HSAG’s analysis includes a comprehensive review of treatment limitations every three years with an attestation-based review during the subsequent years.
The following table highlights the MHP activities conducted by HSAG:
For questions related to the Mental Health Partiy activity, please contact:
Stacy Wittkamper, MPA, LSW
Project Manager II, Medicaid Services
Telephone: 602.801.6507
Email: SWittkamper@hsag.com
Oregon Medicaid EQRO
- Compliance Monitoring Reviews
- Fraud, Waste, and Abuse Reviews
- Performance Improvement Projects
- Network Access Evaluations
- Performance Measure Validation
- Information Systems Capability Assessments
- Annual Technical Report
- Encounter Data Validation
- Mental Health Parity
- Contact Us
- Abbreviations and References


